Neurofeedback helps treat attention deficit disorder, anxiety, depression, and drug addiction. It is often called “biofeedback on steroids” because it provides a more efficient way to get the brain into shape than traditional biofeedback does.
Neurofeedback (also called EEG biofeedback) uses computers and sensors to track and give feedback on brain wave activity. The patient learns to control the patterns of their brain waves, usually with the help of a therapist or coach. Here are a few things to know about neurofeedback therapy for trauma before opting for it:
1. It Works Like a Guided Meditation for the Brain
Like traditional biofeedback, neurofeedback often takes relaxation techniques and combines them with real-time EEG data to give patients immediate feedback about their mental state.
Experts use this form of therapy to train the brain and manage responses and reactions to different stimuli. Neurofeedback therapy is often used with cognitive-behavioral therapy (CBT) to treat trauma.
2. It Can Reduce Traumatic Memories
People recovering from post-traumatic stress disorder (PTSD) often experience anxiety, depression, intrusive thoughts, and flashbacks when certain stimuli trigger them. These thoughts can take a toll on their relationships, work, and psyche.
Neurofeedback can help reduce the severity of these symptoms by teaching the brain not to overreact to triggers. This therapy has even been shown to improve memory recall in people with PTSD, which could also help reduce traumatic flashbacks.
3. It’s Not Just for Adults Who Have Experienced Trauma
Neurofeedback is also used to reduce the symptoms of attention deficit disorder (ADD), attention deficit hyperactivity disorder (ADHD), and autism.
Children with these conditions often exhibit impulsivity, short attention spans, and difficulty staying in their chairs during class. Parents can use neurofeedback to monitor their child’s brainwave activity in real time and help them learn to control their focus.
4. It Often Involves Meditation and Affirmation Exercises
Neurofeedback therapists usually teach patients how to meditate or use self-affirmation before they begin the process of neurofeedback itself. These techniques help them understand what they are trying to accomplish during this time, making it easier for the patient and therapist to see the results in the data.
5. Expensive and Time-Intensive
The NeuroCranial Restructuring process, which uses neurofeedback to increase blood flow in the brain, can take several months before any improvement is noticeable. This therapy often involves 50 sessions or more that must be completed consecutively to experience results.
6. Might Take More Than One Session to Work
This therapy can take several sessions to start working, so it is impractical for people who only have one session per week. It may also be challenging to make progress if the patient isn’t ready to open up about their traumatic experience or lacks confidence in their ability to relax and control their thoughts.
It depends on how severe the trauma symptoms are and how much they have been practicing to control their brainwaves. Patients who come in for neurofeedback therapy often do so after other methods have failed them.
Trauma Therapy: Talking Might Not Be Enough
Trauma therapy, traditionally centered on talk therapy, acknowledges the profound impact of traumatic experiences on individuals’ mental and emotional well-being. Verbalizing trauma can be a crucial step in the healing process, offering a safe space for individuals to express and process their emotions. Talk therapy provides a platform for validating emotions, helping patients recognize that they are not to blame for the traumatic events they endured. It fosters a sense of understanding and empathy, reinforcing the idea that their reactions are valid responses to extraordinary circumstances.
Additionally, talk therapy serves as a powerful tool for reframing the traumatic event. Therapists guide individuals in looking at their experiences through a new lens, helping them gain insight, understanding, and a sense of empowerment. By providing a narrative framework, talk therapy aids in reshaping the way individuals perceive and make meaning of their trauma, paving the way for psychological healing. Moreover, the therapeutic relationship established through talk therapy creates a sense of community, care, and support. This supportive environment is crucial for individuals to feel heard, understood, and connected, promoting a healing journey that encompasses both the emotional and psychological aspects of trauma recovery.
How Does Trauma Affect the Brain and Body?
How Does Trauma Change the Brain?
Trauma induces significant changes in the brain’s structure and function. The amygdala, responsible for processing emotions, becomes overactive in response to trauma, heightening emotional reactions and fostering feelings of fear and anxiety. The prefrontal cortex, vital for decision-making and emotional regulation, may undergo alterations, affecting an individual’s ability to manage emotions effectively. Additionally, the trauma’s impact on the hippocampus, crucial for memory functions, can result in difficulties with memory recall and the processing of traumatic events. These neurological changes collectively contribute to challenges in emotional regulation, decision-making, and memory, emphasizing the intricate ways in which trauma shapes the brain. Understanding these transformations is essential for designing targeted interventions that address both the psychological and neurological aspects of trauma recovery.
“The Body Keeps Score”: Trauma & the Body
“The Body Keeps the Score,” a phrase popularized by psychiatrist Bessel van der Kolk, underscores the profound connection between trauma and the body. It encapsulates the idea that traumatic experiences are not only stored in memories but also imprinted in physical sensations. Trauma can manifest as chronic pain, tension, and other somatic symptoms, emphasizing the intricate interplay between psychological and physiological aspects of the trauma response.
Recognizing that the body serves as a repository for trauma, therapeutic approaches are increasingly incorporating somatic interventions. Techniques such as yoga, mindfulness, and body-centered therapies aim to address and release the physical manifestations of trauma, promoting holistic healing. “The Body Keeps the Score” highlights the importance of acknowledging and treating the somatic components of trauma for a more comprehensive and effective recovery.
New Treatments for Calming the Brain & Body After Trauma
In the journey of recovering from trauma, cutting-edge treatments are paving the way for a holistic approach that addresses both the mind and body. Unlike conventional therapies, these new treatments recognize that trauma goes beyond just words, delving into the physiological realm. One such promising solution gaining traction is neurofeedback therapy. This non-invasive technique actively involves individuals in regulating their brainwave patterns, fostering a sense of calm and emotional equilibrium. With a focus on holistic healing, these advancements signify a shift towards comprehensive well-being, acknowledging the interconnected nature of mental and physical recovery after trauma. Explore these innovative approaches for a more integrated and effective path to healing.
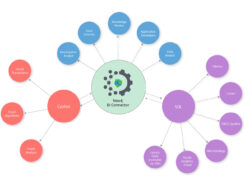
What is Neurofeedback Therapy?
Neurofeedback therapy is a non-invasive technique that aims to regulate brain activity. It involves real-time monitoring of brain waves, with individuals learning to self-regulate and optimize their neural patterns.
Does Neurofeedback Therapy Help with Trauma? What’s the Evidence?
Research suggests that neurofeedback therapy can be beneficial in trauma recovery. By promoting self-regulation, it may help individuals modulate their emotional responses and alleviate symptoms associated with trauma.
What Types of Neurofeedback Therapy Are Helpful for Trauma or PTSD?
1. ILF (Infra-Low Frequency) Training for Trauma:
ILF training targets the slowest brainwave frequencies, associated with deep states of relaxation. This approach aims to calm the nervous system, offering a foundation for trauma survivors to regain a sense of safety.
2. Alpha-Theta Training for Trauma:
Alpha-theta training encourages a state of deep relaxation and enhanced creativity. This can be particularly beneficial for those grappling with traumatic memories, facilitating a more detached and less distressing perspective.
Wrapping Up
Nowadays, neurofeedback therapy for trauma can be a valuable tool in the recovery process. However, it might not replace traditional therapies or medication. It can complement them by helping patients manage their symptoms and behaviors before reaching a crisis point.
Also Read: What Should You Know Before Going for Radiation Therapy?
Frequently Asked Questions:
- Does neurofeedback treat trauma?
A: Yes, neurofeedback is recognized as a promising therapeutic approach for trauma. Training individuals to regulate their brainwave patterns, aims to alleviate symptoms, promote emotional balance, and contribute to overall trauma recovery. - What is the best treatment for complex trauma?
A: The optimal treatment for complex trauma often involves a multi-faceted approach. Integrative therapies like trauma-focused cognitive-behavioral therapy (TF-CBT), Eye Movement Desensitization and Reprocessing (EMDR), and dialectical behavior therapy (DBT) have shown effectiveness. Tailoring the treatment to individual needs, along with a supportive therapeutic relationship, is crucial for comprehensive healing. Consultation with mental health professionals can guide the selection of the most suitable treatment plan. - What is the best therapy for healing trauma?
A: There isn’t a one-size-fits-all answer. Therapies like EMDR, CBT, and DBT are commonly effective. However, the best therapy depends on individual needs and preferences. A strong therapeutic relationship and a trauma-informed approach are key factors in successful trauma healing. Consultation with a mental health professional helps determine the most suitable therapeutic path. - How many neurofeedback sessions are typically needed for trauma?
A: The number of neurofeedback sessions for trauma varies. Generally, individuals may undergo 20 to 40 sessions, but the exact duration depends on the severity of the trauma and individual response. Regular assessments with a qualified practitioner help tailor the treatment plan for optimal results.